“Every day we respond, and we attach ourselves to the worst day of somebody’s life.” [see Phil Melnychuk, “Online program gives firefighters some advance notice about the trauma and tragedy they’ll face”, Delta Optimist, March 20, 2024]
That’s the way Captain Ben Lewis recently described the
nature of a firefighter’s job. Extracting a car crash victim, saving multiple
lives at a fentanyl overdose scene, recovering the charred body of a child from
a house fire. Attending the worst day of somebody’s life every day, day after
day, can take its toll on firefighters and other first responders serving our
communities.
The apparent rise in mental injuries
First responders are not the only workers at risk of mental
or psychological injuries. Many workers’ compensation jurisdictions and
work-disability insurers have noted increasing mental disorder (also called psychological
injury, mental injury) claims over time.
In this post, we survey some of the data reflecting this
increase. We will explore some of the
reasons for the increase. In a later post, we will look more closely at the
drivers behind current trends. We will
also discuss some of the challenges in
comparing data across jurisdictions and prevention strategies that might impact
the trajectory of future trends.
Important note on Terminology
This is intended as a general discussion document and will
use several different terms. This requires
a caution with respect to terminology.
Certain terms may carry negative connotations, confer a
sense of blame, or infer a flaw in an individual. The terms used in this post are
reflect the terms most often used in diagnostic, policy, coding, statistical
and legislative data being discussed.
Psychological injury, mental disorder, mental illness, mental
impairment, mental health injury, and other terms used here often have specific
meaning or legal definitions that apply to in specific jurisdictions. There are also other terms that I have not used
in this discussion but may be included in the categories discussed here. For
example, operational stress injury and military sexual trauma are terms
specific to certain armed forces. Legislation, policy, and coding standards use
various terms to address this topic.
Similar terms in different jurisdictions may or may not carry the exact
meaning or definition.
In the general context of work-related claims, my preferred
terms are “psychological injury” and “mental
health injury” . Mental health
condition, mental health injury, psychological injury, mental health challenge,
and similar terms are used in cited material.
Diagnosis or criteria in the
DSM-5-TR, ICD-11, and equivalent classification systems are not
always the same as those used in practice, policy, or legislation. Certain mental health disorders including
PTSD do appear in these references and generally have specific meanings that
are consistent across jurisdictions but may not be consistently applied or
reflected in statistical reports. This variation in terms makes
interjurisdictional comparison more difficult.
Tracking mental injury statistics in Workers’ Comp and
Disability Insurance
Workers’ compensation recognition of the relationship
between work and psychological injury, particularly in the absence of physical
trauma, has lagged the scientific acceptance. Where short and long term disability (STD and
LTD) insurance or social security disability insurance plans (SSDI in the US) are
available, they are often accessed before (or instead of) filing a workers’ compensation claim. The threshold for
STD, LTD and SSDI is “disability” from employment while workers’ compensation claims
must first establish a work-related cause before considering the issue of
disability.
The Canadian data [from the Association of Workers’
Compensation Boards of Canada – National Work Injury Statistics Program]
reflect a rising trend in accepted work-related
mental disorder claims (7,378 in 2022). While the overall trend in work-related
time-loss injuries was declining (at least until the COVID-19 pandemic),
time-loss claims involving mental disorders or syndromes have trended upward.
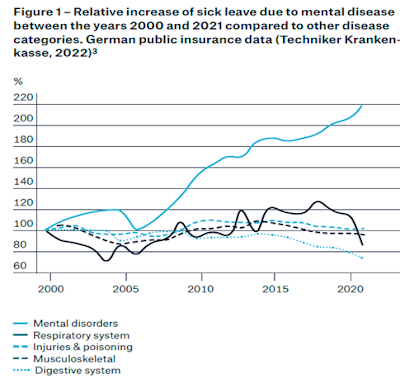
The shape of the
index line for mental health conditions in the Australian data reminded
me of a Munich Re study that looked at the relative increase in sick leave due
to mental disease over a similar period, [See Munich Re, Mira Risk Review:
Munich Re’s Mental Health Calculator, 2022 at https://www.munichre.com/content/dam/munichre/contentlounge/website-pieces/documents/MunichRe-MRRP-Menthal-Health-Calculator_en.pdf] Munich Re notes:
"Mental health
conditions are an increasing challenge globally, but most noticeably in
industrialized countries.
… the rise in incidence is reflected in higher numbers of
life insurance applicants disclosing mental diseases as well as increased
numbers of claims
…most mental health conditions are considered chronic or
recurrent and have a high correlation with other health issues, despite good
treatment.
…complexity in managing mental health conditions is the
rule, rather than the exception.”
"
Sun Life Canada reports 24% of all new short-term disability (STD) claims and 32% of new long-term disability (LTD) claims are for mental illness. The greater complexity and longer duration of these claims account for a disproportionate 45% of claim costs. (See SunLife, Changing Times: evolving the approach to disability management, 2021 at Changing times: evolving the approach to disability management | Sun Life).
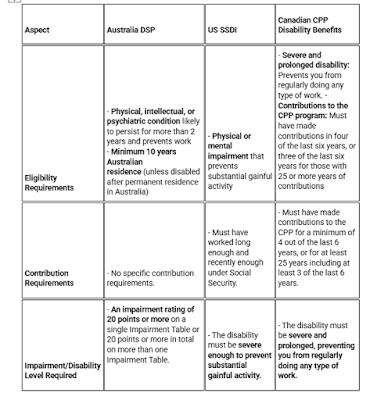
Social Insurance mental injury data
Social insurance generally covers a wider population than workers’ compensation but may reflect trends that are felt by workers’ compensation and disability insurance. The following table highlights aspects of the Australian Disability Support Pension (DSP), US Social Security Disability Insurance (SSDI), and Canada Pension Plan – Disability.
US Social Security provides benefits to workers for certain disabilities. Looking only at the subset of Social Security Disability Insurance (SSDI) for workers who have filed for workers’ compensation or public disability benefits, musculo-skeletal diagnosis dominate. Note, however, that the diagnostic categories involving mental disorders are significant:Changes in coding definitions make a time series using this
subset of SSDI data difficult but it appears that the representation of mental
disorders in this subset has fallen between 2010 and 2022. Looking only at this medical category of SSDI
claims, and using only table 34 in the Annual Statistical Report on the Social
Security Disability Insurance Program for each year, the combination of “Depressive,
bipolar, and related disorders” or “Mood
Disorders” with the “Other” category have fallen from about 14.1% (2010) to 9.3%
(2022) of beneficiaries who have filed for workers' compensation or public
disability benefits.
The Canada Pension Plan Disability (CPP-D) system covers
persons with contributions to the plan who suffer a “severe and prolonged”
disability. Unlike in the US SSDI, I
could find no data isolating just those who had also filed workers’
compensation claims. The following are
based on December counts of benefit cases paid each year 2011(325,620 cases)-2023
(305,679 cases) and isolating mental disorders and all other classes of principle
diagnosis :
Australia Department of Social Services (DSS) provides data
on the demographics of Disability Support Pension (DPS) recipients quarterly. I’ve
selected December data reports and created an index by primary medical condition
isolating the psychological/psychiatric category and all others (excluding the
psychological / psychiatric category):
About 37% of the total
783,625 case were included in the Psychological/psychiatric category in 2023,
up from about 33% in 2015.
I could not find a study quantifying overlaps and possible
substitution of sick leave, social insurance for workers’ compensation mental
injuries. It is possible that workers’ compensation and other forms of
disability compensation (including employer provided sick leave, short-term
disability, and long-term disability) are experiencing similar patterns.
These data suggest mental disorders are a significant issue
for workplace participants, workers’ compensation, social insurance and disability
insurance plans.
Mental Injuries Are Not Always Associated with Physical
Trauma
Most workers encounter a workers’ compensation claim because
of work-related physical trauma. Mental injuries and disorders may well develop
following physical injury, but that is not always the case. SafeWork Australia
found that more than half of mental disorder serious injury claims arose from
work-related harassment, bullying, and workplace pressure.
Safe Work Australia,
Data insights - Snapshot: Psychological health and safety in the
workplace, February 2024
The Canadian data illustrate the distribution of claims by
the nature of the disorder. Post-traumatic Stress Disorder (PTSD) tops the list
but occurs in combination with other disorders and physical injuries. With
PTSD, adjustment disorder, stress, and anxiety contribute to making up the
majority.
While the
range of descriptions noted is wide, recall that these data are for accepted
time-loss claims. That means the
adjudicative authority has determined the work-relatedness of the loss. Many cases of a similar nature may be denied
for mental disorders or injuries. More
on the standard and burden of proof in
the next part of this series.
Employees
with employer provided or employee group
plans for short or long-term disability may seek coverage through those plans.
As noted in earlier posts, many STD and LTD carriers will require claimants to
file claims with workers’ compensation or social insurance plans as a condition
of coverage under LTD or STD.
Who
suffers mental disorder injuries?
The following table lists the top 15 Canadian time-loss claims coded for mental disorders by occupation (Minor grouping level, first four digits of National Occupational Classification- Canada) by the number of accepted time-loss claims from 2020 to 2023:
Please note
that most of these occupations have something that might not be immediately
obvious: high levels of unionization. This
may contribute to greater awareness of health and safety issues as well as
better advocacy supports that contribute to greater success in claim filing. The relatively lower numbers of accepted
mental disorder claims among retail clerks may be more reflective of lower
levels of unionization than lower exposure to harms.
Australian workers’ compensation data are grouped more by industrial sector but
reflect a similar industrial distribution. The “Public administration and
safety industry” includes police services, investigation and security services,
fire protection, other emergency services, and correctional and detention
services. The following figure appears in Safe Work Australia’s data report on “Psychological
health and safety in the workplace”:
How Representative Are These Data?
Both the Canadian and Australian workers’ compensation data
have gaps and inconsistencies that likely understate the extent of work-related
mental disorders in the workplace. Data
for all jurisdictions in either country are not reported in all years. There are no corrections or adjustments for
changes in legislation that may occur over reported periods of time. So, these data may not fully represent what
is happening in either country’s workers’ compensation system.
Direct comparisons between countries are further complicated
by differences in classification systems and coding practices. At best, these data likely reflect broader
trends.
That said, trends for individual jurisdictions over time are
further complicated by changes in definitions, interpretation, diagnostic
methods, adjudicative practice, mix of industries, and a host of other issues within the jurisdiction. Factors such as growing recognition of the
reality of work-related mental injuries and declining stigmatization of mental
disorders will likely impact reported claims but are difficult to assess.
To be clear, work-related mental injuries are real and despite
the shortcomings in the available data, what we have available provides a good indication
the reality of work-related mental injury is being somewhat (if not fully)
recognized.
Whether because of physical injury, a complication of
treatment, or work-place conditions, workers are being harmed. That harm is
significant and as life-altering for the bullied construction worker as it is
for the burned-out air-traffic controller or the PTSD afflicted first
responder.
Summary
Data from multiple sources show:
·
Mental disorders are a significant issue for
workers’ compensation, disability insurers and social insurance entities
·
Increasing proportion of workers’ compensation
claims in at least some jurisdictions
·
Increasing associated costs
Next time
These data on of
mental disorders demonstrate the significance of the issue. They also illustrate some of the key
challenges in comparing data across jurisdictions.
In Part 2, we will explore some of the differences in the
determination of claim acceptance in workers’ compensation programs and
consider initiatives for prevention and treatment.